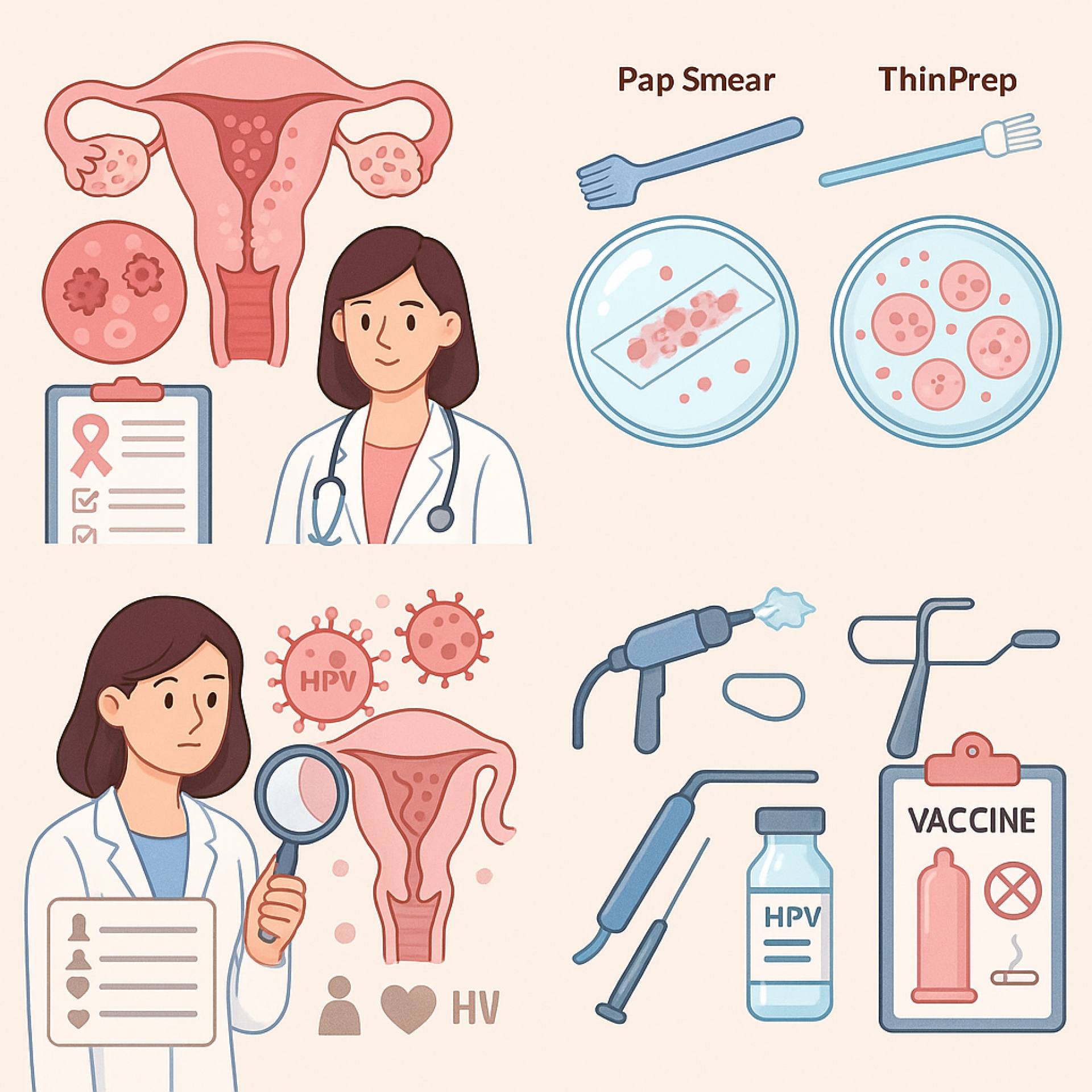
Cervical Cancer Screening (Pap smear, ThinPrep): Early Detection, Timely Treatment
Cervical Cancer Screening (Pap smear, ThinPrep): Early Detection, Timely Treatment
Clitoria Clinic Sexual Health & Pelvic Exams, Phetkasem 81, Bangkok
Friendly doctor, private and inclusive environment, open-minded, attentive, non-judgmental.
Article by Dr. Thitipon Tungwiwatthanapanit :
General Practitioner, Sexologist, Founder of Clitoria Clinic
Cervical cancer screening is a highly effective method
for detecting abnormal cervical cells in the early stage
to prevent progression to cervical cancer
one of the most common cancers among Thai women.
Research by the World Health Organization (WHO)
and the American Cancer Society
confirms that regular Pap smear or ThinPrep testing can detect abnormalities early
and allow effective treatment, significantly reducing mortality rates.
Cervical Cancer Screening with Pap Smear and ThinPrep
Pap smear and ThinPrep involve collecting cells from the cervix
and examining them under a microscope
to check for cell changes,
which may result from HPV (Human Papillomavirus) infection.
ThinPrep is a newer technique
in which the sample is collected and preserved in liquid,
resulting in clearer cell images
and reducing the chance of missing abnormal cells.
Differences Between Pap Smear and ThinPrep
- Pap Smear
- Cells are collected from the cervix and smeared directly on a slide, then stained and examined under a microscope.
- This method has been used for a long time but may have overlapping cells or contamination with mucus or blood.
- Results may be less clear due to these factors.
- ThinPrep
- Cells are collected and placed in a preservative solution.
- Debris is removed, leaving only the cells needed for examination.
- This improves accuracy of results.
- The same sample can also be tested for HPV.
How Often Should You Screen?
- Pap smear: every 1 year
- ThinPrep or HPV co-testing: every 2-3 years if results are normal
Who Should Get Cervical Cancer Screened?
- Women aged 21 and above, even without sexual experience
- All women who have been sexually active
- Those with multiple partners or partners at high sexual risk
- Those with a history of HPV infection or abnormal results
- Those with weakened immunity, e.g., HIV-positive individuals
Causes of Cervical Cell Abnormalities
- HPV infection, especially types 16 and 18, strongly linked to cervical cancer
- Smoking, which increases cell mutation risk
- Weakened immunity (e.g., HIV infection)
- Early sexual activity or multiple partners, increasing HPV exposure risk
- Family history of cervical cancer
Warning Signs of Cervical Cancer
Early-stage cervical cancer usually has no symptoms, but advanced disease may present with:
- Abnormal vaginal discharge, foul smell, or blood-stained discharge
- Bleeding after intercourse or between periods
- Chronic pelvic pain, unexplained weight loss
Diagnosis of Cervical Cancer
A doctor collects cervical cells with a spatula or brush for laboratory testing. If abnormalities are detected, further testing may include colposcopy and biopsy to confirm diagnosis.
Treatment of Cervical Cancer
- For pre-cancerous cell changes (CIN13): cryotherapy or LEEP (Loop Electrosurgical Excision Procedure)
- For cancer: surgery, chemotherapy, or radiotherapy, depending on stage
Prevention of Cervical Cancer
- Regular Pap smear or ThinPrep every 3 years (ages 21-65)
- HPV vaccination
- Condom use during every sexual encounter
- Avoid smoking
Regular screening detects abnormalities at the pre-cancer stage,
giving almost a 100% cure rate.
Dont wait for symptoms get screened early.
- ThinPrep cervical screening: 1,490 THB
- HPV test 14 high-risk types: 1,290 THB
- HPV test 29 types: 2,590 THB
(Prices above exclude doctors fee)
- ThinPrep + HPV 14 types + pelvic exam by doctor: 2,590 THB
- HPV Vaccine 3 doses : 15,990 THB
Consult our medical team at Clitoria Clinic, Phetkasem 81
Tel: 081-116-3788 | LINE OA: @dr.clitoria
Meta Description: Pap smear and ThinPrep cervical cancer screening detect early-stage disease, prevent progression, and protect womens health.
Keywords: Pap smear, ThinPrep, cervical cancer, pelvic exam, HPV, cancer prevention